Ringworm (dermatophytosis) is a common fungal infection of hair, skin, or nails. Image source: The US Centers for Disease Control and Prevention
 Geneva: The World Health Organization (WHO) has issued its first-ever comprehensive report addressing the alarming shortage of medicines and diagnostic tools for invasive fungal diseases. The report, released today, emphasizes the urgent need for enhanced research and development (R&D) to fill these critical gaps, particularly as fungal infections continue to rise globally, affecting vulnerable populations.
Geneva: The World Health Organization (WHO) has issued its first-ever comprehensive report addressing the alarming shortage of medicines and diagnostic tools for invasive fungal diseases. The report, released today, emphasizes the urgent need for enhanced research and development (R&D) to fill these critical gaps, particularly as fungal infections continue to rise globally, affecting vulnerable populations.
These infections, including those caused by Candida, which leads to conditions such as oral and vaginal thrush, are growing increasingly resistant to treatment. These infections are of particular concern for individuals with compromised immune systems, such as those undergoing chemotherapy, living with HIV, or having received organ transplants. As global health experts warn, the lack of effective treatments and diagnostics has made it difficult to manage and treat invasive fungal infections, leading to preventable deaths.
Dr. Yukiko Nakatani, WHO Assistant Director-General for Antimicrobial Resistance ad interim, stressed the severity of the situation, stating, “Invasive fungal infections threaten the lives of the most vulnerable, but countries lack the treatments needed to save lives. The pipeline for new antifungal drugs and diagnostics is insufficient, and there is a void in fungal testing, especially in low- and middle-income countries. This diagnostic gap means that the cause of people’s suffering remains unknown, making it difficult to get them the right treatments.”
The report covers systemic antifungal drugs in development worldwide, including label extension and repurposed products, and critically evaluates how well the current pipeline addresses infections caused by WHO fungal priority pathogens.
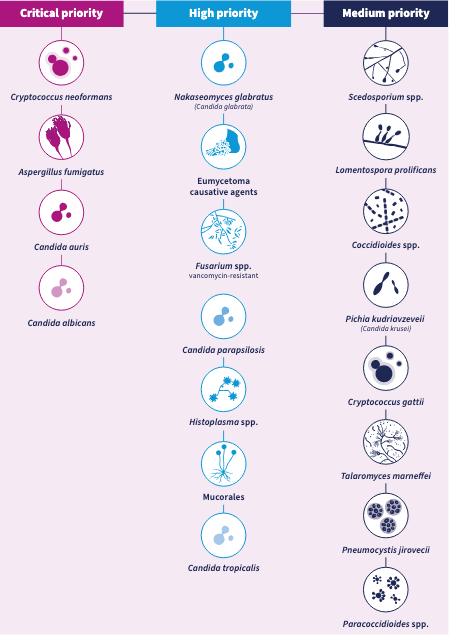
The WHO’s fungal priority pathogens list (FPPL) categorizes the most dangerous fungi responsible for invasive infections. With mortality rates as high as 88%, these pathogens present a significant public health risk, particularly as advancements in medical treatments increase the number of people living with immunocompromised conditions. Invasive fungal diseases are expected to rise as immunocompromised populations grow, further complicating the global health response.
WHO fungal priority pathogens list
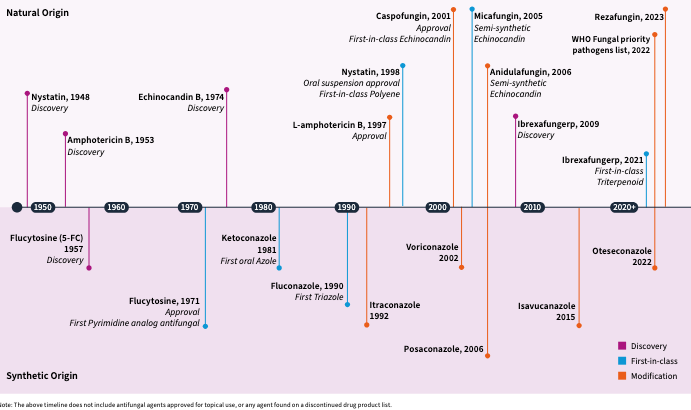
The report provides an in-depth review of the drugs that are being developed to target these critical pathogens. In the past decade, only four new such drugs have been approved by regulatory authorities in key global regions, including the United States, the European Union, and China. Presently, nine such drugs are in clinical development to address the most critical fungal pathogens, but only three of them are in phase 3, the final stage of clinical trials. This limited progress means that few new treatments are expected to be approved in the next decade. Additionally, 22 drugs are still in preclinical development, which is insufficient to ensure a steady pipeline for addressing these diseases.
A significant challenge with current drugs is the range of serious side effects, frequent drug interactions, limited dosage forms, and the necessity for prolonged hospital stays. The report highlights the urgent need for safer treatments, which could help reduce the requirement for continuous drug monitoring, making treatment more accessible and less burdensome.
Historical overview of systemic antifungal drugs and their marketing authorization
The report on these drugs also calls attention to the particularly vulnerable group of children who are underserved by existing antifungal treatments. Few clinical trials have focused on pediatric dosing or age-appropriate formulations. WHO has recommended the expansion of clinical research for pediatric antifungal treatments to better address the needs of young patients.
The report underscores the urgent need for new treatments, as the current antifungal drug pipeline remains insufficient to meet the rising demand for effective treatments, particularly in low- and middle-income countries (LMICs). These regions often lack the necessary diagnostic tools, medications, and infrastructure to manage these infections effectively.
Diagnostic Shortages in Low-Resource Settings
In addition to the scarcity of effective treatments, the WHO report on diagnostics highlights the significant gap in available tools to identify these infections. While commercially available tests exist for some fungal pathogens, they often require well-equipped laboratories and highly trained personnel, making them inaccessible in many low- and middle-income countries (LMICs). These regions, which are the hardest hit by invasive fungal infections, particularly need affordable, fast, and accurate diagnostic tools that can be used at or near the point of care.
Existing diagnostic tests are often inaccurate, slow, and only able to detect a limited range of pathogens. These tests are also often unsuitable for primary and secondary healthcare facilities in low-resource settings, as they require stable electricity and specialized equipment. In addition, many health workers are inadequately trained to recognize and address fungal infections, particularly in areas where resistance is increasing. The result is a lack of proper diagnosis and inappropriate treatment for affected patients.
WHO’s diagnostics report calls for the development of more efficient and affordable diagnostic tools that can be used in a variety of settings, particularly in areas where resources are limited. This would significantly improve early detection and treatment, saving countless lives and reducing the spread of resistant fungal infections. WHO also emphasized the need to enhance global surveillance efforts and strengthen the health workforce’s capacity to manage these infections.
The WHO report calls for a global response to invasive fungal diseases and antifungal resistance. Specifically, it urges increased investment in surveillance, the expansion of financial incentives for drug discovery and development, and the funding of basic research to identify new targets for antifungal medicines. WHO is also developing an implementation blueprint for the FPPL to guide global efforts in combating these infections and improving treatment outcomes.
The report underscores the need for urgent action to address the growing threat posed by these infections, which are increasingly resistant to treatment. WHO’s call to action includes not only improved diagnostics and newmedicines but also increased education and training for healthcare workers, particularly in regions most affected by these diseases.
As the global health community continues to grapple with the growing burden of such diseases, WHO’s groundbreaking report highlights the need for a concerted effort to close the treatment and diagnostic gaps that are undermining efforts to save lives and prevent the further spread of resistant fungal infections. With global collaboration, there is hope for developing better treatments and diagnostic solutions for invasive fungal diseases, which remain a critical public health challenge.
– global bihari bureau