
COVID-19 Notes
 By Dr. Satish K Gupta*
By Dr. Satish K Gupta*
Why did herd immunity not work for COVID-19?
More than 10.1 billion doses of vaccine have already been injected word over. Nearly 61.7% world’s population has been vaccinated with at least one shot. And more than 416 crore people have received full vaccination by both doses. But COVID-19 refuses to go from the world. The contagion continues to haunt even the countries with more than 90% vaccination coverage like the UAE. Why? What happened to herd immunity? Where are we heading to?
Principle of herd immunity?
Herd immunity, or (Community immunity), is said have kicked in when a large cohort of the population in an area becomes immune to a pathogen, and that level of societal protection is able to contain further spread of disease. The concept of herd immunity is based on the principle that the microbes use susceptible hosts to travel in society. When with widespread effective vaccination, hardly any people are left in society to carry the infection forward, even the vulnerable remain shielded from the disease, then the Herd Immunity is said to have set in. So in the herd, while not every single individual is immune, the group as a whole gets an umbrella of protection. The infection rates drop, and the disease wanes off.
When does a community is said to have acquired herd immunity?
It happens when a specific percentage of the population becomes immune to the disease either by vaccination or by infection. Depending upon its transmissibility percentage threshold required may vary for every pathogen.
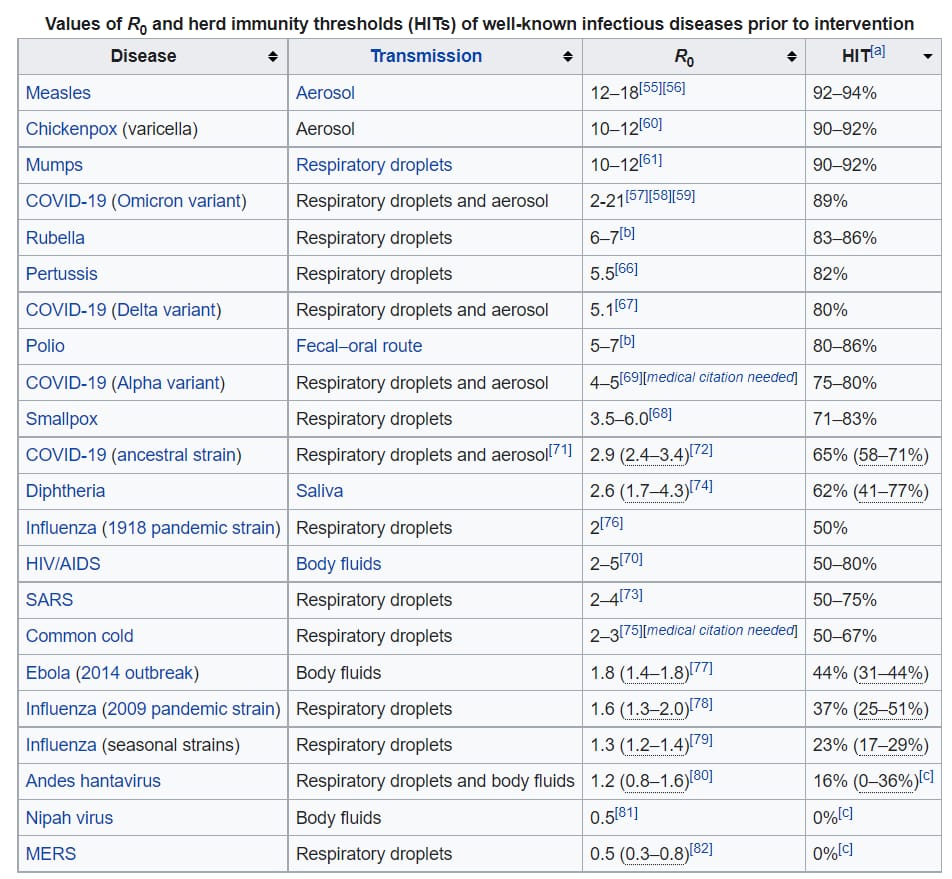
Microbes with higher transmission rates would obviously need a larger percentage of the immune population to be contained. For example, herd immunity against measles requires about 95% of the population to be vaccinated. For polio, the threshold is about 80%.
How do scientists calculate the herd immunity threshold?
Herd immunity depends upon the reproduction number or R0. The R0 is the average number of people that an infected person can further infect if those people aren’t already immune. The higher the R0, the more people need to be resistant to reach herd immunity.
Why did herd immunity experiments fail for COVID -19?
Because the virus has been constantly evolving to more and more transmissible variants. The original Wuhan virus had an R0 of 2.9 requiring about 65% immune population. But soon the virus changed to the alpha version which had R0 of 4-5 demanding a percentage of 75-80%. Further evolution of virus in Delta avatar had R0 of 5.1 and in late 2021 came the Omicron with a sky high R0 of 10 -21, requiring immunization of more than 90% of population.
Why is herd immunity not working for countries like India despite more than 95% seropositivity?
Herd immunity requires permanent robust immunity. The immune resistance of individuals against Sars CoV-2 in society is going down either by virtue of waning vaccine effectiveness (especially mRNA vaccines) or evolving virus has been overriding the existing immunity. Studies showing that boosters are important in preventing symptomatic infection suggest that vaccine effectivity is going down.
Can WHO’s call for vaccination of more than 70% of world population set in herd immunity?
WHO sets a target for all countries to vaccinate 10% of their populations by the end of September. 56 countries effectively excluded from the global vaccine marketplace were not able to reach this target – and most of them in Africa.
With vaccine inequality many countries are at risk of missing the WHO targets of vaccinating 70% of the population of every country by the mid of this year 2022. Though a composite figure of vaccination 70% of world population is likely to be achieved within a month with current rates of vaccination, the figure may remain far from being achieved for certain African nations.
But mass vaccination would still be effective.
Recent observations amply clarify that vaccines protect from severe disease, hospitalization and death. Further mass Vaccination may be able to protect the world from emergence of newer variants.
So mass vaccination may not have been a gurantee of immunity from disease but definity a surity of safety from death.
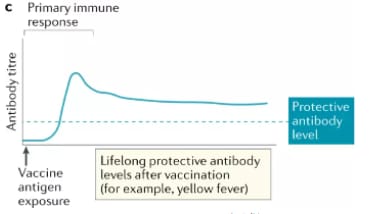
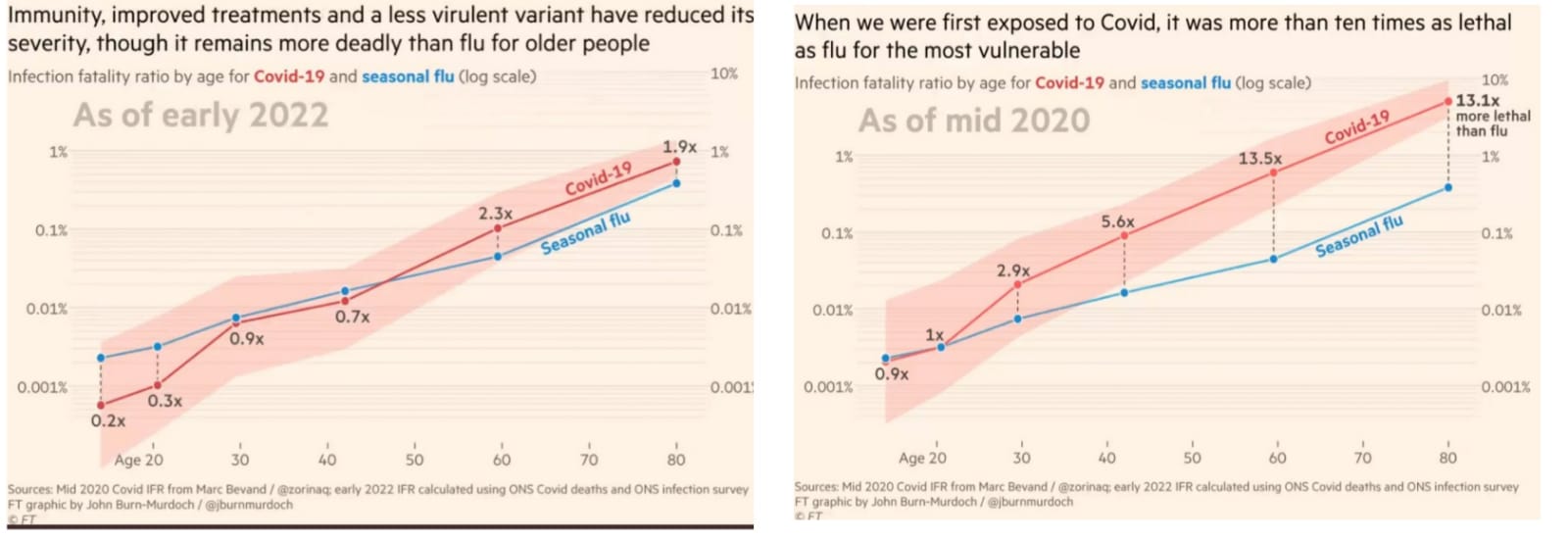
The interplay of virus and vaccines may not have been able to achieve herd immunity but has significantly brought down mortality from Covid-19. In fact, current vaccines have been able to tame the virus to the level of Flu with similar case fatality rates.
Why we are not able to achieve herd immunity from Covid -19?
Vaccines produce three types of immunity:
1. Local Mucosal Immunity in form of IgA antibodies which block the entry of the pathogen and are important in curtaining the speed of transmission. We know present Covid-19 vaccines don’t induce local mucosal immunity and hence don’t protect from infection, so the pandemic is likely to continue unless we have effective vaccines that are able to break the chain of transmission even for the future variants. Nasal vaccines remain the hope of future.
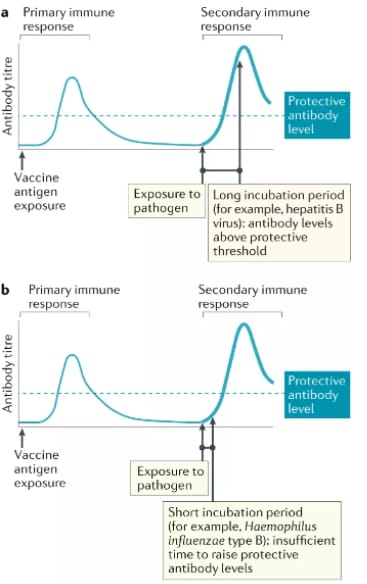
2. Humoral Immunity: IgG antibodies, most commonly talked about immunity, also easy to measure by widely available tests. Certain diseases like Measles and Yellow Fever maintain the specific antibody level and hence herd immunity. But in Covid-19 the antibody levels drop within 4 to 6 months of vaccination requiring the booster dose so Herd immunity doesn’t set in.
3. Long term Cellular Immunity: Conferred by patrolling T cells that are crucial in long-lasting protection. With are no commercially available tests to measure the same remain most elusive to document in most research papers. This immunity takes about 7 to 10 days time to mount an immune response as the time taken in the production of a fresh crop of antibodies after the antigenic challenge. The decrease in the number of severe cases and falling mortality rates against Omicron may be attributed to this arm of the immune system. But how long his protection remains effective in case of Sars Cov-2 will be known with time. As, *even this arm of immune response is vulnerable to being rendered ineffective in case the virus evolves to a variant with a very short incubation period mounting quick complications even before T cells are able to kick in production of antibodies against fresh challange of virus.
Should people take repeat doses of the Covid-19 vaccine?
Recommendations are based on evidence, protecting life is most important and repeated doses are not new among vaccines. Afterall we give two shots against measles during childhood, more than Five doses for DPT and multiple jabs are given against tetanus – now recommended one every 10 years for adults.
In the same way, some way countries are now giving out a third or even fourth dose of the COVID-19 vaccine in the space of a little over a year after studies showed that vaccine effectiveness was waning.
With harder to achieve herd immunity for Covid-19, it is all the more every individual’s responsibility to stay protected and safe by following scientific guidelines. With evolving experience and understanding recommendations may change but till then bear the blanket of frequent vaccination*.
Also read:
- It is time for a universal Corona vaccine
- India sees 40% weekly rise in deaths; WHO to prioritise study of new Omicron lineage BA.2
*Dr. Satish K Gupta is an MD in Medicines, a Visiting Senior Consultant Physician and Internist at Max Super Speciality Hospital, and a Clinical Assistant Professor at GS Medical College, Chaudhary Charan Singh University, Meerut. He is the author of Journey of COVID in India: A Doctor’s Perspective.





Really interesting post!