COVID-19 Notes
 By Dr. Satish K Gupta*
By Dr. Satish K Gupta*
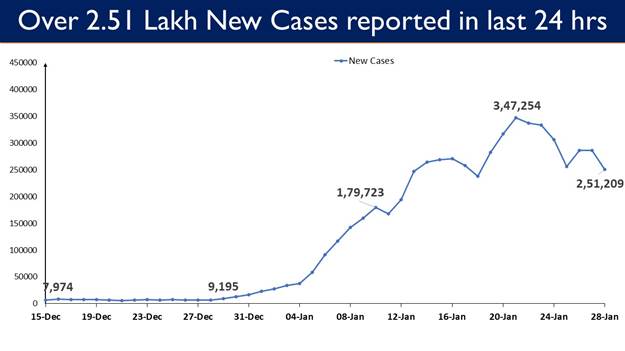
COVID-19 Updates
- 2,51,209 new cases recorded in the last 24 hours till 9 am today
- Daily positivity rate (15.88%)
- Weekly Positivity Rate (17.47%)
Since the start of the pandemic in December 2019, the SARS-CoV-2 has mutated multiple times, giving rise to different variants. Most vaccines were designed to recognize the original SARS-CoV-2 spike protein, newer versions of virus like Omicron have developed potential at escaping protection offered by the vaccines, although they still prevent severe disease.
Every time a new variant comes along, COVID-19 vaccine makers have to reassess neutralization potential of existing vaccines to see if they work against an evolving virus—like Omicron, which has spread quickly around the globe within a month. Pfizer has already started tweaking its vaccine using Omicron specific Spike protein.
When current vaccine can be updated against Omicron, what is the need for Universal vaccine?
It’s pretty clear that the virus continues to evolve and Omicron is not the last variant so going forward there would be a need for a universal COVID-19 vaccine or even a universal coronavirus vaccine.
Who is funding the Universal Covid Vaccine?
Research efforts to accomplish this ambitious project are being supported by the National Institutes of Health ($ 46 million) and Coalition for Epidemic Preparedness ($200 million) – a non-profit organization based in Oslo, Norway.
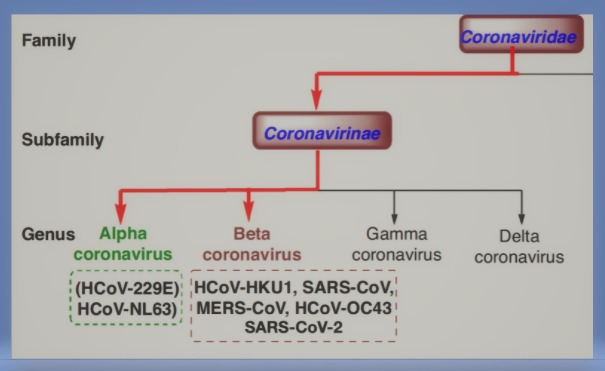
Before we talk of various technologies to make the universal vaccine, let’s first know the deadly family
There are four families, or genera, of coronaviruses: alpha, beta, gamma, and delta. All seven coronaviruses known to infect humans belong to either the alpha or beta families. The beta family has been more dangerous for humans:
- The two in the alpha family, 229E and NL63, both cause common colds.
- Beta family includes
-
- two common cold viruses, OC43 and HKU1,
-
- as well as all three viruses that have caused deadly outbreaks in humans: SARS-CoV-1, SARS-CoV-2 and MERS-CoV.
-
What is the biggest difficulty in making a universal vaccine against corona viruses?
What are the genetic diversity that exists among the alpha beta gamma and delta the various branches of Corona family?
How the scientists wish to overcome the challenge?
Most research groups have zoomed in on the beta coronaviruses—and, more specifically, a subgroup known as sarbecoviruses that includes SARS-CoV-1 and SARS-CoV-2, which are more genetically similar to one another than to MERS-CoV, OC43, or HKU1.
Which Institutes are working on universal vaccine?
1. Walter Reed Army Institute of Research USA, is way ahead and farthest in development of a universal vaccine which has already been found successful in animal studies and tested in humans as part of a Phase I trial. Vaccine is now being tested in the lab against Omicron.
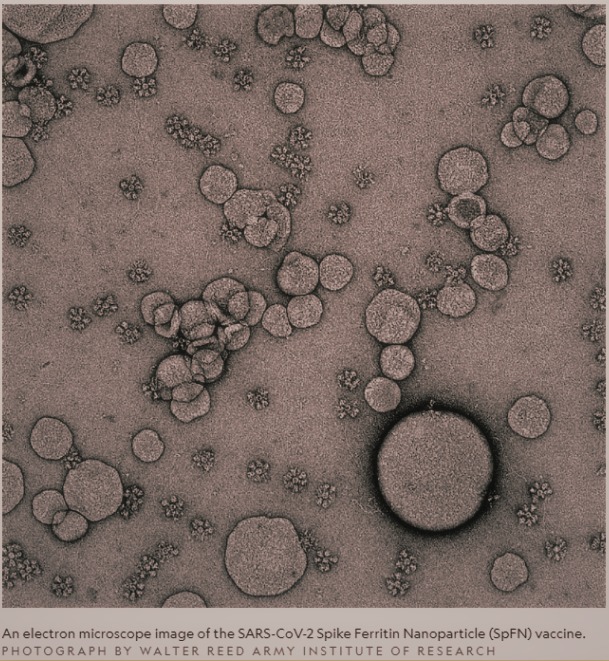
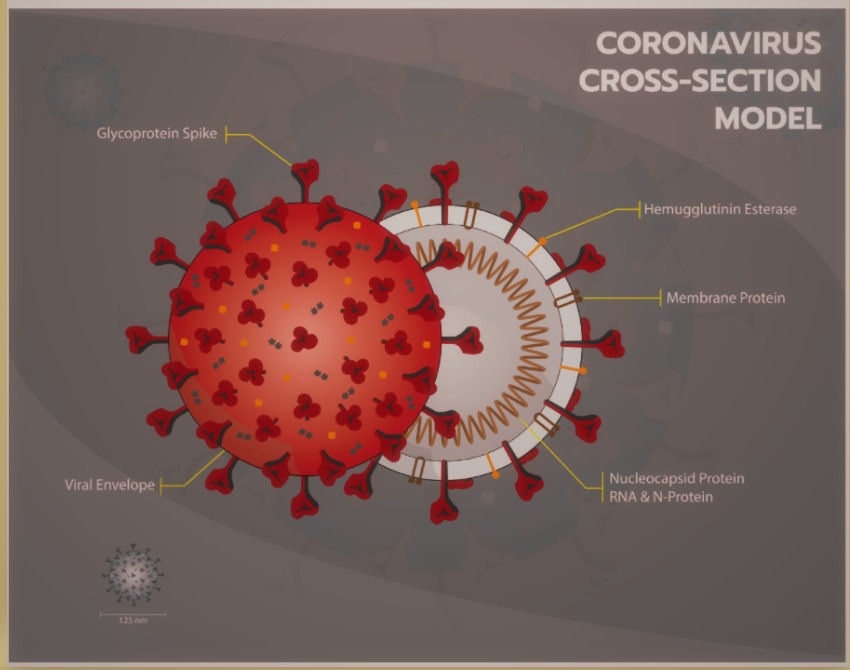
Walter Reed’s Spike Ferritin Nanoparticle COVID-19 vaccine, or SpFN, Uses a foot ball-shaped nanoparticle with 24 faces studded with multiple copies of the *original SARS-CoV-2 spike protein. The repetitive and ordered display of the coronavirus spike protein on a multi-faceted nanoparticle stimulates immunity in such a way as to translate into significantly broader protection.
2. California Institute of Technology: Mosaic vaccine of eight different Corona Viruses – Researchers at Caltech used RBD proteins from up to eight viruses, including the original SARS-CoV-2 and other SARS-like coronaviruses isolated from bats, that were fused onto a nanoparticle with 60 faces. Early animal experiments have shown that vaccine stimulated production of diverse antibodies, which blocked infections caused by several SARS-like viruses, including coronavirus strains not used to create the vaccines.
3. Duke Human Vaccine Institute: To make a pan-SARS-like virus vaccine, Institute focusing on a very specific part of the RBD, common in most corona viruses. Vaccines induces development a potent antibody dubbed DH1047 against the specific part of the RBD. Monkey experiments proved vaccine’s ability to protect against not just SARS-CoV-2 but several other coronavirus infections.
4. University of Washington: University of Washington is working to tap potential of T cells. As antibodies are very specific to one type of variant—but for a pan-coronavirus vaccine it may be better to engage the T cell response. Because unlike antibodies, T cell responses actually recognize parts of the virus that get broken down inside the cell.
5. Northwestern University Feinberg School of Medicine: Penaloza-MacMaster, group is working on a vaccine that expresses both the spike protein and other segments of SARS-CoV-2—such as the nucleocapsid, an internal protein that is more conserved among viruses than the spike protein.
6. Other institutes: Brigham and Women’s Hospital in Boston and the University of Wisconsin, Madison.
The need for at least a pan-SARS-like coronavirus vaccine cannot be ignored. Hence the challenges posed by fast changing Sars Cov-2 are being looked with sincerity.
Though the development of a Universal Corona Virus vaccine may not be an easy task but an honest beginning has been made. Hope that a safe and effective pan-corona vaccine providing life-long immunity soon becomes a reality.
Masterpiece: “I don’t want anyone to think that pan-coronavirus vaccines are literally around the corner in a month or two,” Anthony Fauci. Current vaccines dramatically reduce the risk of hospitalization and severe illness, even against new variants like omicron. And crucially, they are available today.
Also read:
*Dr. Satish K Gupta is an MD in Medicines, a Visiting Senior Consultant Physician and Internist at Max Super Speciality Hospital, and a Clinical Assistant Professor at GS Medical College, Chaudhary Charan Singh University, Meerut. He is the author of Journey of COVID in India: A Doctor’s Perspective.