More evidence supports increased transmissibility of the Delta variant of COVID-19
Geneva/New York City: Despite efforts to extend vaccination coverage, many countries across all regions continue to experience surges in COVID-19 cases.
A 12% increase in global new cases of COVID-19 were reported between July 12-18, 2021 as compared to previous week, with over 3.4 million new cases. Almost 57 000 deaths were reported last week, a similar number to the previous week, following a steady decline in the number of deaths for over two months. Cumulative number of over 190 million cases and more than 4 million deaths reported globally.
An increase in global COVID-19 case weekly incidence, with around 490 000 cases reported each day compared to 400 000 in the previous week, were reported.
During the period the highest numbers of new cases were reported from Indonesia (350 273 new cases; 44% increase), the United Kingdom (296 447 new cases; 41% increase), Brazil (287 610 new cases; 14% decrease), India (268 843 new cases; 8% decrease), and the United States of America (216 433 new cases; 68% increase).
According the the World Health Organization (WHO), the increases in transmission appear to be driven by four factors: the circulation of more transmissible Variants of Concern (VOCs), relaxation of public health social measures originally intended to control transmission, increases in social mixing, and the large number of people who remain susceptible to SARS-CoV-2 infection as a result of inequitable vaccine distribution around the world.
“Vaccine inequity is the world’s biggest obstacle to ending this pandemic and recovering from COVID-19,” said Dr Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization. “Economically, epidemiologically and morally, it is in all countries’ best interest to use the latest available data to make lifesaving vaccines available to all,” he said.
COVID-19 vaccine inequity will have a lasting and profound impact on socio-economic recovery in low- and lower-middle income countries without urgent action to boost supply and assure equitable access for every country, including through dose sharing, according to – the Global Dashboard for COVID-19 Vaccine Equity, a joint initiative from the United Nations Development Programme (UNDP), the World Health Organization (WHO) and the University of Oxford’s Blavatnik School of Government, which combines the latest information on COVID-19 vaccination with the most recent socio-economic data to illustrate why accelerating vaccine equity is not only critical to saving lives but also to driving a faster and fairer recovery from the pandemic with benefits for all. It shows that an acceleration in scaling up manufacturing and sharing enough vaccine doses with low-income countries could have added $38 billion to their GDP forecast for 2021 if they had similar vaccination rates as high income countries.
The new data released today shows a high price per COVID-19 vaccine dose relative to other vaccines and delivery costs – including for the health workforce surge – could put a huge strain on fragile health systems and undermine routine immunization and essential health services and could cause alarming spikes in measles, pneumonia and diarrhoea. There is also a clear risk in terms of foregone opportunities for the expansion of other immunization services, for example the safe and effective rollout of HPV vaccines. Lower income countries need timely access to sustainably priced vaccines and timely financial support.
“In some low- and middle-income countries, less than 1 per cent of the population is vaccinated – this is contributing to a two-track recovery from the COVID-19 pandemic”, said UNDP Administrator, Achim Steiner. “It’s time for swift, collective action – this new COVID-19 Vaccine Equity Dashboard will provide Governments, policymakers and international organizations with unique insights to accelerate the global delivery of vaccines and mitigate the devastating socio-economic impacts of the pandemic,” Steiner added.
“Closing the vaccine gap is required to put this pandemic behind us. The dashboard can help scale up and accelerate global delivery of vaccines by providing accurate, up-to-date information on not just how many vaccines have been given, but also the policies and mechanisms through which we get them into arms,” said Dr. Thomas Hale, Associate Professor of Global Public Policy, Blavatnik School of Government, University of Oxford.
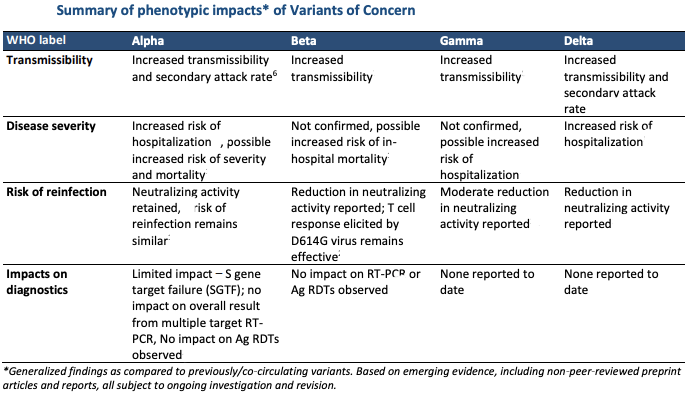
In the meantime, WHO’s latest figures show that globally, cases of the Alpha variant have been reported in 180 countries, territories or areas (hereafter countries; six new countries in the past week), while 130 countries (seven new countries) have reported cases of the Beta variant; 78 countries (three new countries) have reported cases of the Gamma variant; and 124 countries (13 new countries) have reported cases of the Delta variant.
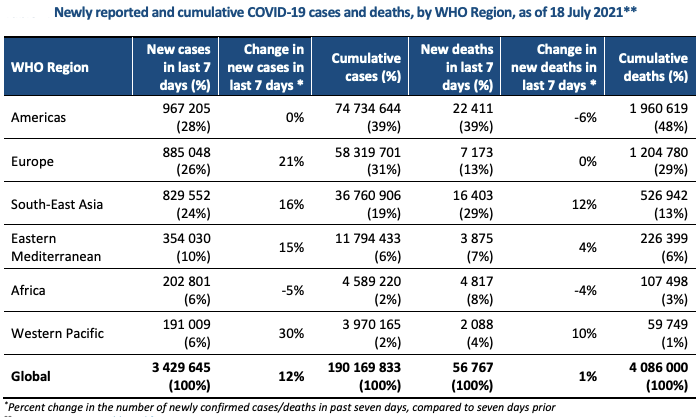
The number of deaths increased in the WHO’s South-East Asia (that also includes India) and the Western Pacific Regions by 12% and 10%, respectively, as compared to the previous week. The African, Eastern Mediterranean and European Regions reported similar numbers of deaths as compared to the previous week, whereas the Region of Americas reported a 6% decrease.
The Region of the Americas and the European Region reported the highest weekly case incidence per capita, both reporting 95 new cases per 100 000 population, as well as the highest number of deaths per population over the past week, with 2.2 and 0.8 new deaths per 100 000 population, respectively. The Eastern Mediterranean and South-East Asia Regions reported 48 and 41 new cases per 100 000 population, respectively.
WHO stated that over eighteen months into the COVID-19 pandemic, the need for global epidemiological surveillance for COVID-19 continues to be of high importance. “The evolution of transmission patterns as the pandemic continues will likely be influenced by the impact of the COVID-19 vaccination campaigns and by the emergence of more transmissible variants, or variants with properties of immune escape. Timely and complete surveillance data are therefore key to monitoring these changes,” it stated in its latest Weekly Epidemiological Update of July 20, 2021.
Evidence supports increased transmissibility of the Delta variant of COVID-19
Delta and other variants are driving some countries to reinstate strict public health social measures. This is further worsening the social, economic and health impact, especially for the most vulnerable and marginalized people. Vaccine inequity threatens all countries and risks reversing hard won progress on the Sustainable Development Goals.
Growing evidence supports the increased transmissibility of the Delta variant as compared to non-Variants Of Concern (VOC). However, the exact mechanism for the increase in transmissibility remains unclear.
A recent study from China during an outbreak of the Delta variant examined the time interval from the exposure of a quarantined population to the first positive PCR result and found that the interval may be shorter for the Delta variant when compared to non-VOCs [4 (IQR 3.00-5.00) days compared to 6 (IQR 5.00 to 8.00) days, respectively].
Moreover, the viral load of the first positive test of Delta infection was over 1200 times higher than non-VOCs, suggesting that this VOC may be able to replicate faster and be more infectious during the early stages of infection.
A study from Canada analysing data from over 200 000 COVID-19 cases showed an increase in virulence of the Delta variant when compared to non-VOCs. Among the COVID-19 cases, the risk of hospitalization, ICU admission and death associated with the Delta variant compared to non-VOCs increased by 120% (93-153%), 287% (198-399%) and 137% (50-230%), respectively. Increased disease severity was also identified for Alpha, Beta and Gamma variants combined when compared to non-VOCs: 59% (49-69%) for hospitalization, 105% (82-134%) for ICU admission and 61% (40-87%) for death.
Preliminary findings from a study in the United Kingdom, which measured antibodies in a cohort of 112 SARSCoV-2-infected individuals, indicated significantly reduced neutralization titres (2.5 to 5-fold reduction) in sera from individuals infected with Delta, Beta or Alpha variants with a S:484K mutation (but not Alpha without any additional mutations) when compared to the non-VOCs.
Vaccine Efficacy
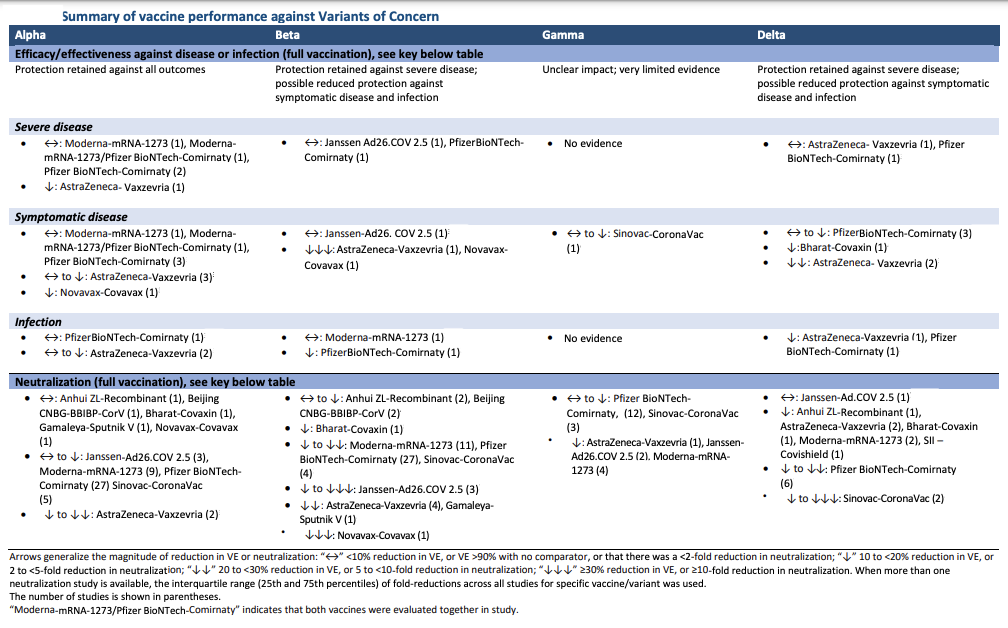
Since July 6, 2021 , two notable studies have provided further evidence of the performance of mRNA vaccines against Alpha and Beta variants.
The first, a test-negative case-control study in the United States of America, found that vaccination with two doses of Moderna-mRNA-1273 or Pfizer BioNTech-Comirnaty vaccines was 92.8% (95% CI: 83.0-96.9%) effective at preventing hospitalization due to the Alpha variant 14 or more days after receipt of the second dose; Vaccine efficacy/effectiveness (VE) against all variants was 86.9% (95% CI: 80.4-91.2%).
It should be noted that approximately 21% of the 1210 adults participating in the study were immuno suppressed.
A second study, from Qatar, evaluated VE of Moderna-mRNA-1273 against SARS-CoV-2 infection and severe disease due to Alpha and Beta variants among a large cohort of adults using a matched test negative case control design. Adjusted VE against infection due to the Alpha and Beta variants 14 or more days after receipt of the second dose was 100% and 96% (95% CI: 90.9-98.2%), respectively. Single dose VE against infection due to Alpha and Beta was reduced: 88.2% (95% CI: 83.8-91.4%) and 68.2% (95% CI: 64.3-71.7%), respectively.
The study also evaluated VE of Moderna-mRNA-1273 against asymptomatic, symptomatic, and severe, critical, or fatal disease due to all variants (predominantly Alpha and Beta). VE of two doses of the vaccine ranged from 90-99% for these outcomes. VE of a single dose remained high for severe, critical or fatal disease (84%) but was markedly lower for asymptomatic and symptomatic disease at 47.3% (95% CI: 37.6-55.5%) and 66.0% (60.6-70.7%), respectively, thus, highlighting the importance of two doses.
– global bihari bureau





