The unvaccinated are many times more at risk of dying from either of the Delta and Omicron variant: WHO
WHO-BROLL Emergencies Coronavirus Press Conference December 29, 2021
Geneva: While the number of recorded deaths caused by COVID-19 doubled from 1.8 million in 2020 to 3.5 million till today and increasing in 2021, the Delta and Omicron variants of the virus are twin threats that are driving up cases to record numbers, which again is leading to spikes in hospitalisations and deaths.
“We know the actual number (of deaths) is much higher,” World Health Organization (WHO) Director-General Dr. Tedros Adhanom Ghebreyesus, acknowledged, adding that this is not to mention to the millions of people dealing with long-term consequences from the virus.
With Omicron being more transmissible, circulating at the same time as Delta, both are leading to a “tsunami of cases”, thus putting immense pressure on exhausted health workers and health systems on the brink of collapse, and again disrupting lives and livelihoods.
WHO further warns that as the pandemic drags on, it is possible that new variants could evade the countermeasures and become fully resistant to current vaccines or past infection, necessitating vaccine adaptations.
However, any new vaccine update would potentially mean a new supply shortage, so it’s important to focus on building up local manufacturing supply to help end this pandemic and prepare for future ones. One way to increase production of lifesaving tools is to pool technology.
WHO pointed out that the pressure on health systems is not only because of new COVID-19 patients requiring hospitalisation but also a large number of health workers are getting sick themselves.
“Omicron is moving so quickly, in addition to vaccination, public health social measures are also needed to stem the wave of infection, protect health workers and systems, open up societies and keep children in school,” Dr. Ghebreyesus said, stressing the need to also treat Mental health as a core element of the response to and recovery from the COVID-19 pandemic.
As the unvaccinated are many times more at risk of dying from either variant, populism, narrow nationalism and hoarding of health tools, including masks, therapeutics, diagnostics and vaccines, by a small number of countries continue to undermine equity, and create the ideal conditions for the emergence of new variants.
92 Member States, out of 194, missed the 40% target set by the WHO for 2021. This was due to a combination of limited supply of vaccines going to low-income countries for most of the year and then subsequent vaccines arriving close to expiry and without key parts – like the syringes!
Besides, in the case of about 20 countries, supply chain and distribution issues to impacted vaccine rollouts.
Moreover, misinformation and disinformation, often spread by a small number of people, have also been a constant distraction, undermining science and trust in lifesaving health tools. WHO contends that in the huge waves of cases currently seen in Europe and in many countries around the world, misinformation which has driven vaccine hesitancy is now translating to the unvaccinated disproportionally dying.
“40% was doable. It’s not only a moral shame, it cost lives and provided the virus with opportunities to circulate unchecked and mutate,” Dr. Ghebreyesus said. He warned: “This virus will continue to evolve and threaten our health systems if we don’t improve the collective response.”
He rued that sharing technology and know-how, as well as waiving the intellectual property rights around COVID-19 tools should have happened early on in the pandemic. “But it’s never too late to come together to do the right thing.”
WHO still hopes to see progress quickly in the New Year. It remains optimistic that this can be the year that not only ends the acute stage of the pandemic but also chart a path to stronger health security. It prescribes that building on the successes and failures nations must not only share vaccines faster and more equitably with COVAX and AVAT, they must support countries in manufacturing and rolling them out to everyone. And access to new treatments must also follow.
The world’s premier health body’s optimism is derived from its past experience of deploying emergency response teams to support governments in their times of greatest need.
WHO’s health emergency system had established an Incident Management Support Team, to run the emergency response and requesting more information about the reports of a cluster of cases of pneumonia of unknown origin in Wuhan, China. Although it had little information, it had enough experience and expertise to know that this looked serious.
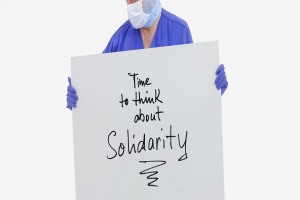
Early on it worked out that beating this new health threat – a new coronavirus potentially capable of spreading quickly around the globe – would require three things:
- Science : to both understand the pathogen
- Solutions: to beating it
- Solidarity: to share and deliver the tools wisely and equitably
And there were major successes that included:
- The rapid development of a comprehensive package of technical guidance on how to ready countries to detect, treat, communicate, and prevent the spread, within two weeks of the first report of the cluster of pneumonia of unknown cause.
- The sharing of the genome, which triggered the development of diagnostics within the first three weeks of 2020.
- A multi-organisational supply chain system was quickly set up, which included solidarity flights, that collectively delivered personal protective equipment for health workers and medical and oxygen supplies for patients.
WHO quickly convened scientists and researchers in January 2020, and regularly thereafter, to develop a research roadmap for COVID-19 that accelerated the science around the virus and the creation of new health tools. This included global solidarity trials on new vaccines and treatments to speed up research and development processes. Thereupon, WHO and partners created the COVID-19 Tools (Act) Accelerator in April 2020 to accelerate access to tests, treatments and vaccines.
Working with clinicians and practitioners around the world, WHO developed a comprehensive living guidance for the clinical management of COVID-19. A common corticoid steroid was found to be effective in cutting the risk of death in those with severe disease in September 2020. The development of new vaccines proved so effective at cutting serious disease and death – they represent a scientific masterclass. The increased level of coordination between WHO and Member States was exemplified by more than 3,500 national regulatory authorizations in 144 Member States, following the approval of vaccines through the WHO Emergency Use Listing.
Dr. Ghebreyesus though stressed that it was also vitally important that the established Scientific Advisory Group for the Origins of Novel Pathogens can develop a pathway for the scientific research of pathogens, including for the origins of SARS-CoV-2. Chalking out a roadmap for 202o, he said he wants governments, industry and civil society to work with WHO on a campaign that targets 70% vaccine coverage in every country by the start of July. “In 2022, WHO will work with our Member States to build well-financed health systems, strengthen preparedness and ensure the equitable distribution of health tools,” he announced.
He also welcomed innovative solutions to reaching vulnerable communities that have not received vaccination yet because the primary doses are the most important for people to develop immunity.
“Bottom-up microplanning with strong community engagement and mobile vaccination teams, which have been highly effective in ridding most of the world of polio, are another way to get vaccines to the hard-to-reach,” he suggested. He announced that WHO will support countries as they look to improve access to COVID-19 tools and catch up with routine immunisation. Besides, he call for leaders of government and industry to walk the talk on vaccine equity both by ensuring consistent supply and helping to get vaccinations actually into people. “Vaccine supply, for now at least, is improving although the emphasis on boosters in rich countries could cause low-income countries to go short again,” he cautioned.
He also called on leaders of rich countries and manufacturers to learn the lessons of Alpha, Beta, Gamma, Delta and now Omicron and work together to reach the 70% vaccination coverage. “This is the time to rise above short-term nationalism and protect populations and economies against future variants by ending global vaccine inequity. I also want to ensure COVID-19 care pathways with new treatments are available in every single country. And to ensure people get on treatment at the optimum time, we need to get tests everywhere,” he said.
Ending health inequity remains the key to ending the pandemic. Setting the agenda for the coming year, he said in 2022, WHO will work with the Member States to build well-financed health systems, strengthen preparedness and ensure the equitable distribution of health tools.
From the new WHO Bio Hub System, which offers a reliable, safe, and transparent mechanism for WHO’s 194 Member States to voluntarily share novel biological materials; to the new WHO Hub for Pandemic and Epidemic Intelligence, based in Berlin – WHO will build mechanisms to enhance partnership.
“In this vein, the development of a new, binding accord between nations on pandemic prevention, preparedness and response, will be a key pillar. I hope to see negotiations move swiftly and leaders to act with ambition,” he said.
– global bihari bureau





