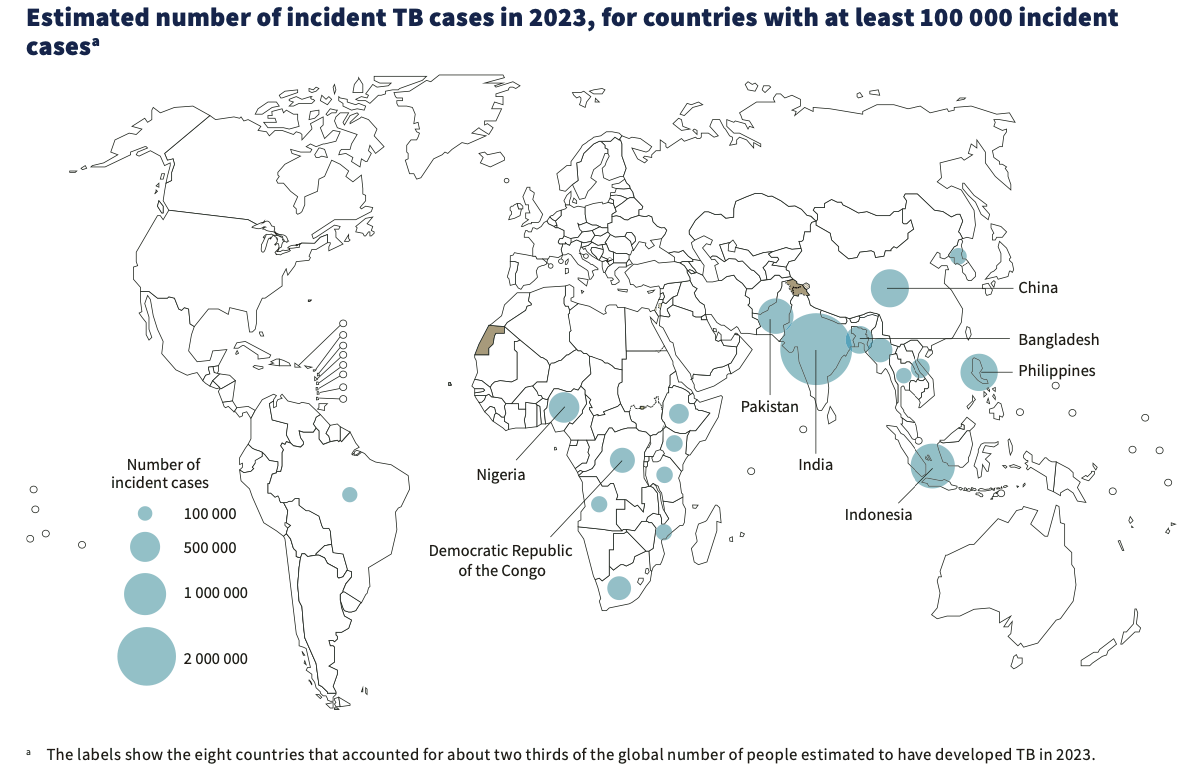
Washington: Tuberculosis (TB) has resurged as the top infectious disease killer with India (26%), Indonesia (10%), China (6.8%), the Philippines (6.8%) and Pakistan (6.3%) together accounting for 56% of the global TB burden.
Most of the people who develop tuberculosis disease each year are in 30 high-burden countries, which accounted for 87% of the global total in 2023, according to a new report on tuberculosis published today by the World Health Organization (WHO).
WHO’s Global Tuberculosis Report 2024 reveals that approximately 8.2 million people were newly diagnosed with TB in 2023 – the highest number recorded since WHO began global TB monitoring in 1995. This represents a notable increase from 7.5 million reported in 2022, placing TB again as the leading infectious disease killer in 2023, surpassing COVID-19.
According to the report, 55% of people who developed tuberculosis were men, 33% were women and 12% were children and young adolescents.
The report highlights mixed progress in the fight against TB, with persistent challenges such as significant underfunding. While the number of tuberculosis-related deaths decreased from 1.32 million in 2022 to 1.25 million in 2023, the total number of people falling ill with TB rose slightly to an estimated 10.8 million in 2023.
“The fact that TB still kills and sickens so many people is an outrage when we have the tools to prevent it, detect it and treat it,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “WHO urges all countries to make good on the concrete commitments they have made to expand the use of those tools and to end TB.”
In 2023, the gap between the estimated number of new tuberculosis cases and those reported narrowed to about 2.7 million, down from COVID-19 pandemic levels of around 4 million in 2020 and 2021. This follows substantial national and global efforts to recover from COVID-related disruptions to TB services. The coverage of tuberculosis preventive treatment has been sustained for people living with HIV and continues to improve for household contacts of people diagnosed with TB.
However, multidrug-resistant TB remains a public health crisis. Treatment success rates for multidrug-resistant or rifampicin-resistant TB (MDR/RR-TB) have now reached 68%. But, of the 400,000 people estimated to have developed MDR/RR-TB, only 44% were diagnosed and treated in 2023.
Funding gaps and challenges
Global funding for TB prevention and care decreased further in 2023 and remains far below target. Low- and middle-income countries (LMICs), which bear 98% of the TB burden, faced significant funding shortages. Only US$ 5.7 billion of the US$ 22 billion annual funding target was available in 2023, equivalent to only 26% of the global target.
The total amount of international donor funding in LMICs has remained at around US$ 1.1–1.2 billion per year for several years. The United States government remains the largest bilateral donor for TB. While the Global Fund to Fight AIDS, Tuberculosis and Malaria (the Global Fund) contribution to international funding of the TB response, especially in LMICs, is important, it remains insufficient to cover essential TB service needs. The report emphasizes that sustained financial investment is crucial for the success of TB prevention, diagnosis, and treatment efforts.
Globally, TB research remains severely underfunded with only one-fifth of the US$ 5 billion annual target reached in 2022. This impedes the development of new TB diagnostics, drugs, and vaccines. WHO continues leading efforts to advance the TB vaccine agenda, including with the support of the TB Vaccine Accelerator Council launched by the WHO Director-General.
Complex drivers of the epidemic
For the first time, the report provides estimates on the percentage of TB-affected households that face catastrophic costs (exceeding 20% of annual household income) to access TB diagnosis and treatment in all LMICs. These indicate that half of TB-affected households face such catastrophic costs.
A significant number of new TB cases are driven by 5 major risk factors: undernutrition, HIV infection, alcohol use disorders, smoking (especially among men), and diabetes. Tackling these issues, along with critical determinants like poverty and GDP per capita, requires coordinated multisectoral action.
“We are confronted with a multitude of formidable challenges: funding shortfalls and catastrophic financial burden on those affected, climate change, conflict, migration and displacement, pandemics, and drug-resistant tuberculosis, a significant driver of antimicrobial resistance,” said Dr Tereza Kasaeva, Director of WHO’s Global Tuberculosis Programme. “It is imperative that we unite across all sectors and stakeholders, to confront these pressing issues and ramp up our efforts.”
Global milestones and targets for reducing the TB disease burden are off-track, and considerable progress is needed to reach other targets set for 2027 ahead of the second UN High-Level Meeting. WHO calls on governments, global partners, and donors to urgently translate the commitments made during the 2023 UN High-Level Meeting on TB into tangible actions. Increased funding for research, particularly for new TB vaccines, is essential to accelerate progress and achieve the global targets set for 2027.
– global bihari bureau