
COVID-19 Notes
 By Dr Satish K Gupta*
By Dr Satish K Gupta*
We still have a lot to learn about Long COVID-19
COVID-19 has settled, the severity of the COVID-19 waves has come down, but Long COVID continues to trouble patients and would be the next health crisis to be battled.
What is Long COVID?
The World Health Organization (WHO) has developed a clinical case definition of the post-COVID-19 condition.
“Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms and that last for at least 2 months and cannot be explained by an alternative diagnosis.”
So Long COVID is a diagnosis of exclusion. The definition may change as new evidence emerges and our understanding of the consequences of COVID-19 evolves.
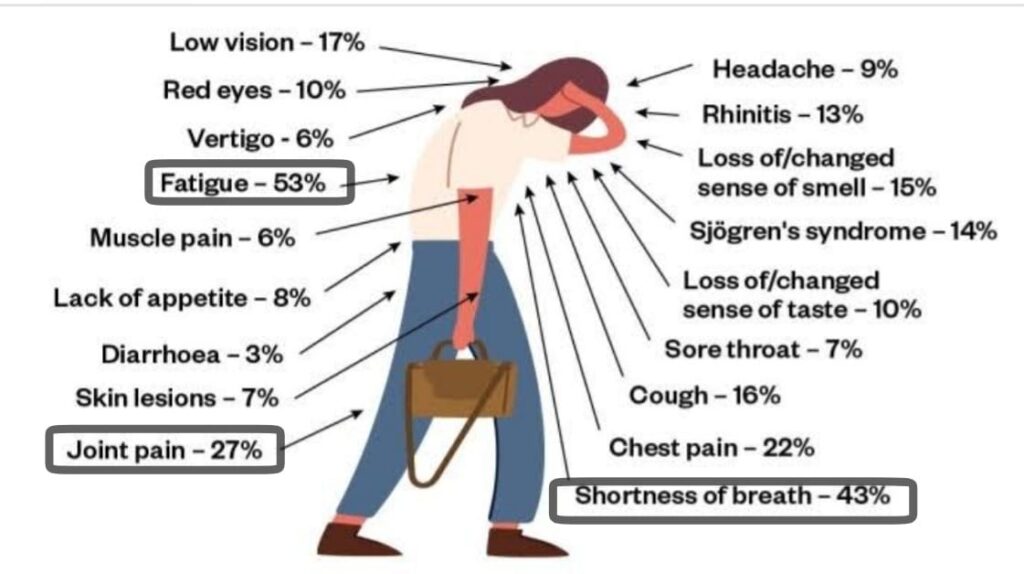
Common Symptoms:
There are more than 200 symptoms listed for Long COVID. But 3 most commonly encountered symptoms affecting the majority of cases are
1. Fatigue
2. Shortness of Breath
3. Fog (Brain Fog)
How severe are the symptoms?
Severity varies from patient to patient but symptoms generally have an impact on everyday functioning.
Do Long COVID patients show fresh symptoms or continued symptoms from the initial disease?
Symptoms may be new-onset following initial recovery from an acute COVID-19 episode or persist from the initial illness. Symptoms may also fluctuate or relapse over time.
What is a common characteristic of post COVID symptoms?
Symptoms frequently get worse after physical or mental activity. The symptoms may affect a number of organs or systems, occur in diverse patterns.
What are the blood tests to diagnose Long COVID?
Long COVID is a condition for which there is currently no standard objective diagnostic test or biomarker. Even raised C-reactive protein (CRP) [made by the liver] may be misleading with variable results in different patients over a period of time. CT scan of the lung can show residual peripheral ground-glass opacities, fibrosis which may improve or worsen over time. Values of d-Dimer may be misleading.
Which patients are more likely to have Long COVID?
Long COVID can affect anyone who had COVID. Cases are reported even after mild or asymptomatic disease. But Long COVID is more commonly seen in women. Obesity, associated co-morbidities like chronic obstructive pulmonary disease (COPD), Diabetes, chronic kidney disease (CKD), autoimmune disorders, immunocompromised states, past history of neuropsychiatric symptoms could be predisposing factors.
Patients who had longer illnesses requiring hospitalization, prolonged ICU stay are more likely to have lingering persistent or recurring symptoms.
Treatment:
1. Fatigue is the most common symptom of Long COVID. Rest, graded exercise and activity limitations are helpful in the majority of cases. Activity goals should be individualised. Non-steroidal anti-inflammatory drugs (NSAID) drugs may be helpful to some patients in alleviating pain. General measures like massage, Vitamin C are often used with variable results. Rest, and adequate sleep are most helpful.
2. Shortness of Breath – It is the most troublesome symptom. The cause of dyspnea must be investigated and treated accordingly. Long COVID associates dyspnea may mostly be a diagnosis of exclusion. Patients with falling SpO2 may require oxygen inhalation. Even 1 to 2 litres of oxygen a few hours a day may suffice. Some patients may be benefitted from the use of Intermittent non-invasive ventilation (BIPAP). Routine use of oral steroids is not indicated for the treatment of Long COVID associated breathlessness. Corticosteroids may be useful early in course of disease in some patients but have limited or no role about six months after the initial COVID. Drugs like Nintedanib and Pirfenidone are often misused and should be left to specialists. Diarrhoea could be a disturbing side effect of these drugs requiring a change of dose or drug.
3. Fog – Brain Fog can present with a variety of symptoms from an inability to think to anxiety nervousness. Reassurance rest and short courses of anxiolytics can help most patients.
Diagnosing and managing symptoms of Long COVID can be tricky, as some symptoms of long COVID-19 overlap with those of other conditions — and people may have a tendency to blame everything on COVID as they recover from the challenging illness.
Prognosis
No one knows what the time duration of Long COVID will be, or what proportion of patients will recover completely or will have long-term symptoms. It may vary from person to person. However, most patients can be helped.
The puzzle still remains unsolved. Many unanswered questions remain a mystery about Long COVID, especially about pathophysiology: Does an autoimmune reaction drive Long COVID? Does the coronavirus linger in reservoirs within the body and reactivate later? What protection against long COVID do vaccines and treatments offer, if any?
To cut long story short, we still have a lot to learn about Long COVID-19. But the reality is that patients suffer and need help. Empathy, reassurance and team approach remains helpful in most of the patients.
With inputs from Dr Arjun Khanna, Senior Consultant, Pulmonology
Also read: India rolls out COVID-19 vaccines for children 12 -14 years of age
*Dr. Satish K Gupta is an MD in Medicines, a Visiting Senior Consultant Physician and Internist at Max Super Speciality Hospital, and a Clinical Assistant Professor at GS Medical College, Chaudhary Charan Singh University, Meerut. He is the author of Journey of COVID in India: A Doctor’s Perspective.





