-
Up to 10 million deaths could occur annually by 2050 due to antimicrobial resistance (AMR), on par with the 2020 rate of global deaths from cancer
-
Pollution in key sectors of the economy contributes to the development, transmission and spread AMR
-
AMR’s economic toll could result in a GDP drop of at least USD 3.4 trillion annually by 2030, pushing 24 million more people into extreme poverty
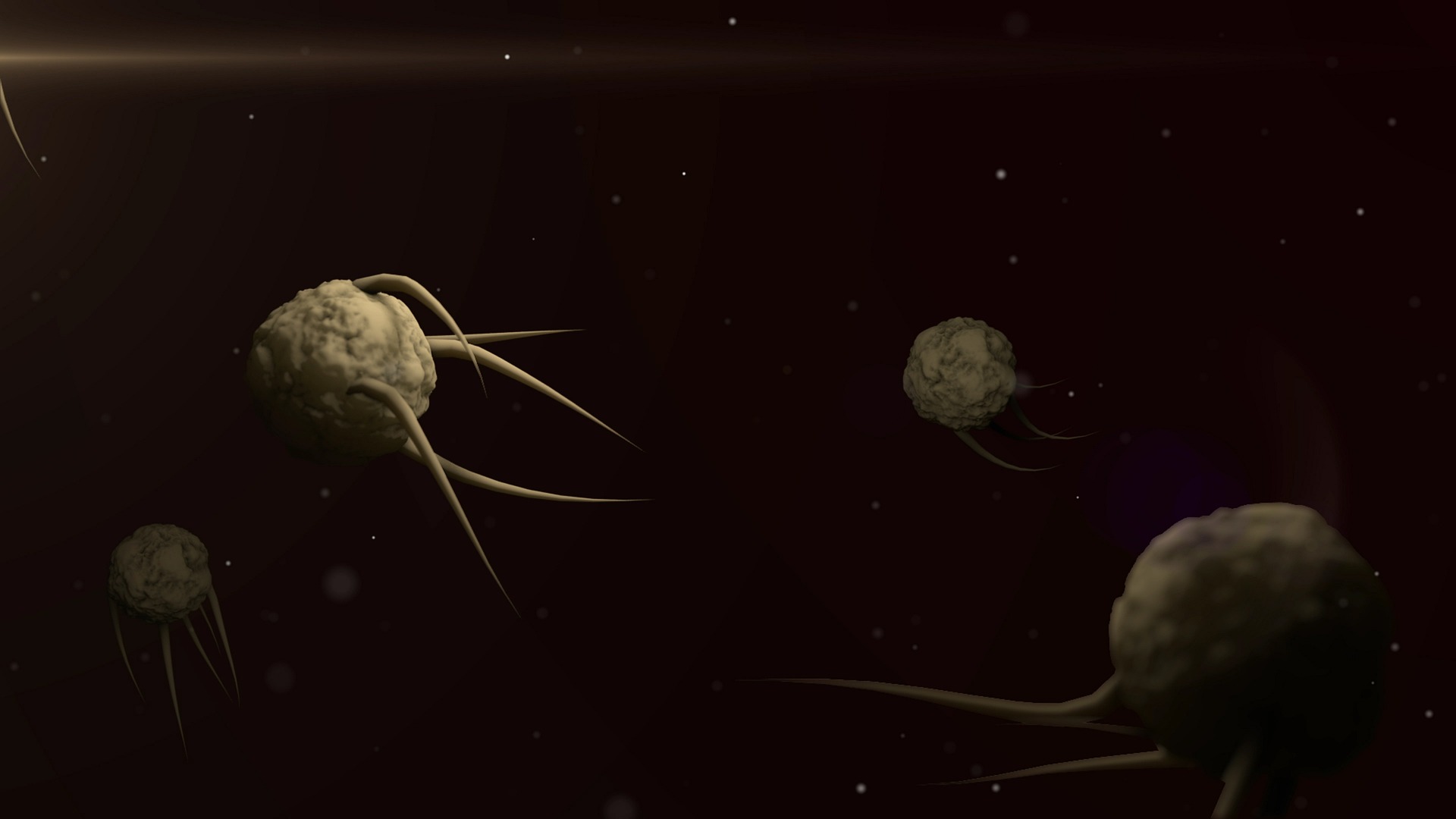
Nairobi: Curtailing pollution created by pharmaceuticals, agricultural and healthcare sectors is essential to reduce the emergence, transmission, and spread of superbugs – strains of bacteria that have become resistant to every known antibiotic – and other instances of antimicrobial resistance, known as AMR. This is the key message of a report released today by the UN Environment Programme (UNEP) on the environmental dimensions of AMR, which already is taking a serious toll on the health of humans, animals, and plants, as well as the economy.
The report, Bracing for Superbugs: strengthening environmental action in the One Health response to antimicrobial resistance was launched at the Sixth Meeting of the Global Leaders Group on AMR, held in Barbados. It calls for a multisectoral One Health response. This is in line with the work of the Quadripartite Alliance, including UNEP, the Food and Agriculture Organization (FAO), the World Health Organization (WHO) and the World Organisation for Animal Health (WOAH).
“The environmental crisis of our time is also one of the human rights and geopolitics – the antimicrobial resistance report published by UNEP today is yet another example of inequity, in that the AMR crisis is disproportionately affecting countries in the Global South countries,” said Prime Minister Mia Amor Mottley, Chair of the One Health Global Leaders Group on Antimicrobial Resistance. “We must remain focused on turning the tide in this crisis by raising awareness and by placing this matter of global importance on the agenda of the world’s nations.”
The development and spread of AMR mean that antimicrobials used to prevent and treat infections in humans, animals and plants might turn ineffective, with modern medicine no longer able to treat even mild infections.
Listed by the WHO among the top 10 global threats to health, it is estimated that in 2019, 1.27 million deaths were directly attributed to drug-resistant infections globally, and 4.95 million deaths worldwide were associated with bacterial AMR (including those directly attributable to AMR).
AMR is expected to cause 10 million additional direct deaths annually by 2050. This equals the number of deaths caused globally by cancer in 2020.
The economic toll of AMR is expected to result in a GDP drop of at least USD 3.4 trillion annually by 2030, pushing 24 million more people into extreme poverty.
The triple planetary crisis entails higher temperatures and extreme weather patterns, land-use changes that alter its microbial diversity, as well as biological and chemical pollution. All these contribute to the development and spread of AMR.
“Pollution of air, soil, and waterways undermines the human right to a clean and healthy environment. The same drivers that cause environmental degradation are worsening the antimicrobial resistance problem. The impacts of anti-microbial resistance could destroy our health and food systems,” said Inger Andersen, Executive Director of UNEP. “Cutting down pollution is a prerequisite for another century of progress towards zero hunger and good health.”
The report highlights a comprehensive set of measures to address both the decline of the environment and the rise of AMR, especially addressing key pollution sources from poor sanitation, sewage, and community and municipal wastes.
To prevent and reduce such pollutants it is crucial to:
- create robust and coherent national-level governance, planning, regulatory and legal frameworks, and establish coordination and collaboration mechanisms
- increase global efforts to improve integrated water management and promote water, sanitation and hygiene to limit the development and spread of AMR in the environment as well as to reduce infections and the need for antimicrobials
- increase integration of environmental considerations into AMR National Action Plans, and AMR into environmental-related plans such as national chemical pollution and waste management programmes, national biodiversity and climate change planning
- establish international standards for what constitutes a good microbiological indicator of AMR from environmental samples, which can be used to guide risk reduction decisions and create effective incentives to follow such guidance
- explore options to redirect investments, to establish new and innovative financial incentives and schemes, and to make the investment case to guarantee sustainable funding, including the allocation of sufficient domestic resources to tackling AMR.
- Environmental monitoring and surveillance and further research prioritization to provide more data and evidence and better target interventions.
AMR requires a One Health response that recognises that the health of people, animals, plants, and the environment are closely linked and interdependent. Prevention is at the core of the action needed to halt the emergence of AMR and the environment is a key part of the solution. Comprehensive and coordinated strengthening of environmental action in the One Health response to AMR will reduce the risk and burden of AMR on humans and nature, as well as help address the triple planetary crisis, UNEP stated.
– global bihari bureau





