
Delhi Government imposes Epidemic Act on Rabies
Global-Standard Public Health Reform or a Panic Reaction?
New Delhi: When the Government of Delhi recently brought human rabies under the Epidemic Diseases Act and declared it a notifiable disease, the move surprised many. Rabies does not spread from person to person. It incubates silently for weeks to months. And tragically, once symptoms appear, survival is almost impossible.
So why deploy epidemic legislation for a disease that does not behave like an epidemic?
The answer lies in epidemiological science — and in lessons already learnt within India and globally. This is not a panic decision. It is a system-level public health reform.
Rabies is biologically unusual. It is not a disease of transmission chains. It is a disease of exposure ecology. It must be defeated before it becomes a disease. The virus enters the body through a bite or scratch, usually from a dog. It then travels silently along nerves for weeks or months before attacking the brain. Once symptoms appear — fever, agitation, hydrophobia, confusion — death is almost certain.
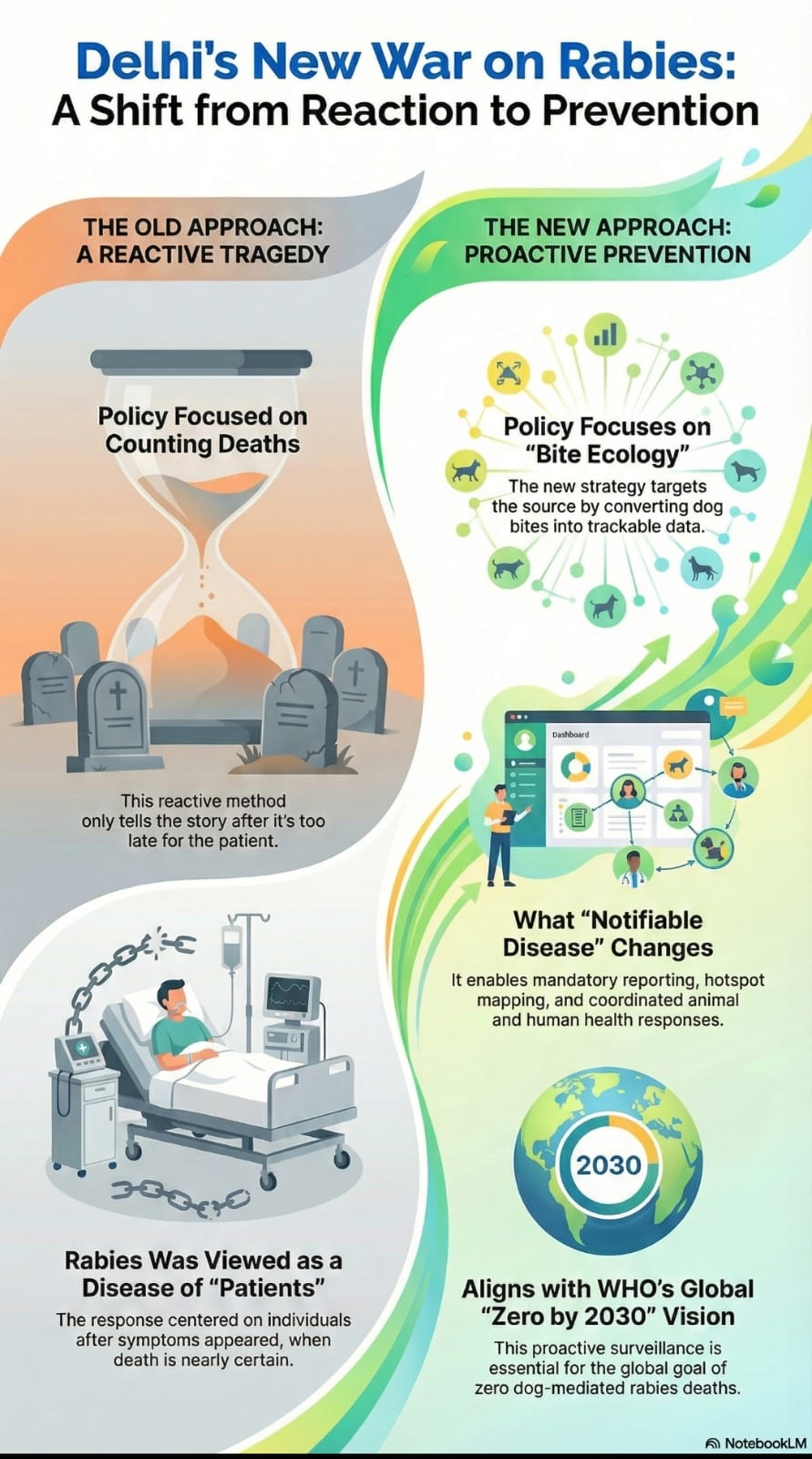
Yet rabies is also one of the most preventable fatal diseases known to medicine. Immediate wound washing, vaccination, and rabies immunoglobulin can prevent nearly every case — if done in time. This means rabies is not really a disease of “patients.” It is a disease of bites.
And that is exactly what Delhi’s new legal classification addresses.
From Death Counting to Bite Ecology
For decades, India’s rabies policy focused on counting deaths. But deaths tell the story too late. Delhi’s move shifts the entire response upstream — to bite surveillance, geographic risk mapping, supply readiness, and animal reservoir control. By making rabies notifiable under the Epidemic Act, Delhi has converted scattered dog-bite cases into real-time biological signals. The street becomes the patient.
What “Notifiable Under the Epidemic Act” Actually Means?
Declaring rabies notifiable means:
• Every government and private health facility must legally report cases
• Bite-related PEP data becomes traceable
• Repeat-bite localities become visible
• Vaccine and immunoglobulin supply planning becomes evidence-based
• Municipal veterinary and animal birth-control teams are activated in hotspot zones
• Enforcement is possible — this is no longer voluntary paperwork
This allows rabies to be governed like tuberculosis, dengue or snakebite — not medically, but administratively.
Indian Precedents: Delhi Is Not Alone
Manipur — Epidemic Act in Action
In the Churachandpur district of Manipur, the Epidemic Diseases Act was invoked in 2025 after rabies cases surged. Containment zones were declared, and administrative controls were imposed to accelerate vaccination drives and control animal reservoirs. This showed that epidemic-law tools can be used for rabies, not for lockdowns, but for coordinated public-health mobilisation.
Jharkhand — Notification and Daily Surveillance
Jharkhand formally declared rabies a notifiable disease and mandated daily reporting by government and private institutions. This shifted rabies from being a “background tragedy” to a tracked public-health condition with enforceable reporting and improved logistics planning.
Meghalaya — Enforcement Frameworks
Meghalaya issued notification orders linking rabies reporting to enforcement provisions — underlining that rabies control needs administrative authority, not only medical advice.
These Indian experiences prove that rabies surveillance improves only when notification is legally binding.
Global Alignment: WHO’s Zero Rabies Vision
The World Health Organization, UNICEF, the Food and Agriculture Organization of the United Nations, and OIE [OIE stands for Office International des Epizooties, which translates to the World Organisation for Animal Health (WOAH) today] have set a global target: Zero human deaths from dog-mediated rabies by 2030.
India carries nearly one-third of the world’s rabies burden.
WHO emphasises that rabies elimination depends on:
• Surveillance of exposures
• Dog vaccination
• One-Health coordination between human and animal health systems
• Guaranteed access to PEP
Delhi’s move fits squarely into this global elimination architecture.
*Why Epidemic Law Was Needed*
Rabies does not need lockdowns. It needs:
• Data discipline
• Legal enforceability
• Coordinated municipal action
• Guaranteed vaccine and RIG supply
• Accountability
Only epidemic-law powers provide this level of coordination and enforceability.
A Rare Case of Policy Matching Biology
Rabies does not spread like influenza — it spreads like geography. Delhi has chosen the correct battlefield: not ICUs and mortuaries, but streets, colonies, schools, markets and waste zones. By converting bites into data, and data into action, Delhi is building India’s first street-level rabies risk radar. It is just not an overreaction. It is a long-overdue epidemiological correction. And it may finally make rabies history.


 By
By 



Perfect Analysis