
Mayotte Dzaoudzi Archipelago
La Réunion/Mayotte: A significant resurgence of chikungunya virus disease is sweeping through the Indian Ocean islands of La Réunion and Mayotte, marking the first major outbreaks in nearly two decades. La Réunion has reported over 47,500 cases and twelve deaths as of May 4, 2025, since widespread transmission began in August 2024. In Mayotte, locally transmitted cases have emerged for the first time since 2005-2006, raising concerns of a similar large-scale outbreak.
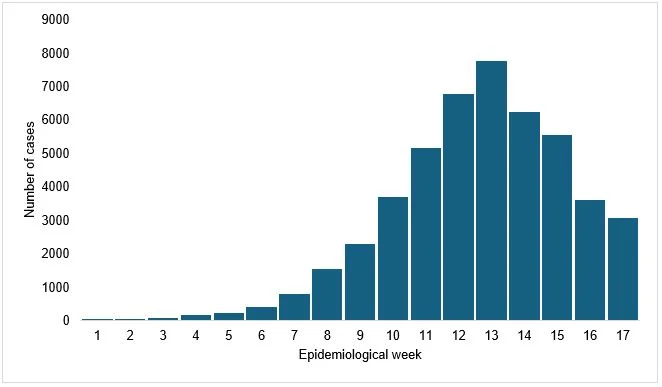
The outbreak in La Réunion escalated sharply in early 2025, with weekly cases soaring from 30 at the end of 2024 to 4,000 in mid-March. While most cases presented mildly, 340 hospitalisations occurred between January 1 and May 4, with older adults and infants being disproportionately affected. Sixty-six severe cases with organ failure have been reported, and twelve deaths in elderly individuals with comorbidities have been linked to chikungunya. An additional 28 deaths, including one neonatal death, are under investigation. The southern municipalities, particularly Le Tampon, are the most affected, though cases have been reported across the island.
Mayotte has reported 116 chikungunya cases as of May 4, including 57 locally acquired, 29 imported, and 30 under investigation. The first local case since the 2005-2006 outbreak (approximately 7,300 cases) was identified on March 26. One hospitalisation has been reported in Mayotte, with no deaths so far. Imported cases linked to travellers from La Réunion have also been reported in Wallis and Futuna and Martinique.
Public health authorities in both La Réunion and Mayotte have implemented response measures. La Réunion activated its ORSEC arboviruses plan, escalating to Level 4 (medium-intensity epidemic) on March 14. Measures include enhanced vector control with additional specialists and increased intervention sites, mosquito net distribution targeting vulnerable groups, mobilisation of national health reserves for vector control and hospital support, and a targeted vaccination campaign for adults under 65 with comorbidities and high-risk professionals. Hospitals have increased bed capacity and established triage systems for chikungunya patients.
In Mayotte, Level 2A of the ORSEC plan was activated on March 26, 2025, with intensified vector control efforts, including the distribution of nets and repellents and insecticide treatments. Hospital capabilities have been reinforced with enhanced diagnostics, surveillance, and infection prevention measures. Public awareness campaigns are also underway.
The WHO said it is actively supporting the affected countries through its Global Arbovirus Initiative, focusing on strengthening healthcare and surveillance capacity, providing guidelines and technical assistance for integrated vector control, increasing laboratory capacity, delivering clinical training to health workers, deploying experts, and providing risk assessment and communication advice.
Chikungunya, transmitted by Aedes mosquitoes, causes fever and severe joint pain. While fatalities are rare, severe disease is more common in the elderly, infants, and those with underlying conditions. The current outbreaks in the Indian Ocean islands, which have a large immunologically naive population and abundant Aedes mosquito vectors, highlight the potential for a significant public health burden. The WHO emphasises the importance of strengthening healthcare, laboratory, and surveillance capacities in all countries, along with vector control and public education, to manage and prevent further outbreaks. While chikungunya vaccines exist, they are not yet widely available. No international travel or trade restrictions are currently warranted.
– global bihari bureau




